2022-11-15
How the immunoproteasome sustains chronic inflammation in COPD
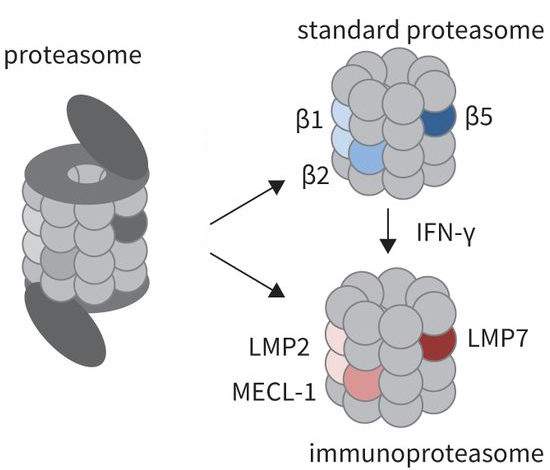
The proteasome (left) consists of a cap structure and a tube made up of various subunits (spheres). The standard proteasome and the immunoproteasome (right) differ in the structure of their subunits. Thus, β1, β2, and β5 of the standard proteasome are replaced by LMP2, MECL-1, and LMP7 in the immunoproteasome. The different subunits cut protein molecules in different ways, thus influencing cell function. Immunoproteasomes are typically present in immune cells, but can also be produced in non-immune cells, particularly under the influence of the messenger molecule interferon-gamma (IFN-γ). (Figure from Kammerl et al., ERJ 2022)
The immunoproteasome affects the persistent inflammation in smokers and those with COPD, making it an interesting target for diagnosis and treatment of the lung disease. This is the central finding of a study published by researchers from the DZL in the European Respiratory Journal.
COPD is characterized by chronic inflammation of the respiratory tract. As immune cells drive this process, they are in focus of many research approaches.
Immune cells have a variety of ways to perceive signals from the environment, allowing them to determine whether there is any threat that needs to be fought off. A previously understudied mechanism in this context is the immunoproteasome, a specialized form of the proteasome that is found only in immune cells. Proteasomes are present in all cells and act as a type of shredder, breaking down no longer needed proteins. Shredded proteins influence cell function in various ways. The immunoproteasome is unique in its structure compared to the standard proteasome (see figure). It plays a central role in immune cell activity and can amplify inflammatory responses.
New insights into the immunoproteasome in COPD
In an article published in the European Respiratory Journal, researchers from the DZL focused on the immunoproteasome, examining how its function is influenced by chronic smoking or severe COPD. To do this, they studied immune cells in the blood, known as mononuclear blood cells. They found that the immunoproteasome was more active in both groups compared to control groups, such as non-smokers or those without COPD. Additional analyses of patients with severe COPD showed that the more activated the immunoproteasome was, the more limited the lung function. Although this is not proof of a direct correlation between the two measurements, in further experiments, the DZL researchers found an interesting indication that this may be the case: when they inhibited the function of the immunoproteasome in blood cells, the release of inflammatory-promoting messenger molecules decreased.
Study provides new starting points for diagnosis and treatment
This observation potentially provides interesting starting points for diagnosis and treatment: by measuring immunoproteasome activity, a so-called biomarker could be developed to indicate the severity of COPD. Regarding treatment, it could be possible to develop drugs that limit the activity of the immunoproteasome, thus reducing inflammation. This could alleviate the symptoms and progression of COPD.
Source: Kammerl IE, Hardy S, Flexeder C, Urmann A, Peierl J, Wang Y, Vosyka O, Frankenberger M, Milger K, Behr J, Koch A, Merl-Pham J, Hauck SM, Pilette C, Schulz H, Meiners S. Activation of immune cell proteasomes in peripheral blood of smokers and COPD patients: implications for therapy. Eur Respir J. 2022 Mar 3;59(3):2101798. Link to the article.
/jbul
/json
Calendar
Upcoming events
2024-04-30
Virtual DZL AID Kick-off Seminar
2024-05-29
74th Meeting of ARCN
2024-06-05
