External link to this publication (open access)
Time lapse movies from the paper
/jbul
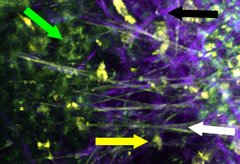
Autofluorescence-based multiphoton microscopy image of a murine trachea displaying epithelial cells (green arrow), immune cells (yellow arrow), collagen connective tissue (black arrow), and elastic fibers of connective tissue (white arrow). (Photo: S. Kretschmer, University of Lübeck)
The range of options is limited when it comes to microscopic examinations inside the human body. This is due to the fact that many dyes used for staining of cells and surface molecules cannot be applied in vivo. Even when some cell types are stainable, the surrounding tissue remains invisible. Scientists of DZL Sites ARCN and UGMLC are working on a technique that circumvents these problems by using so-called autofluorescence, a natural property of cells and fibers. They published their latest results in the August issue of the journal Laboratory Investigation.
Physiological processes of the human body are mostly investigated in model systems, which are not representing the real situation perfectly: First, cells are cultivated in a medium that isn’t equivalent to the tissue environment. Second, interactions between several cell types cannot be investigated in models, because not all of them can be kept in cell culture: Often it’s neither possible to isolate them in sufficient numbers nor to cultivate them over longer time periods. When organoids or animal models are probed by classical methods, this can only be done at just one selected time point. The model system is “stopped” in order to gain information on cellular processes.
Scientists from Lübeck (DZL Site Airway Research Center North, ARCN) and Marburg (DZL Site Universities of Giessen and Marburg Lung Center, UGMLC) developed a microscopic technique for visualizing the structure of airway tissue in collaboration with colleagues from Graz and Jena. They also followed the communication of immune cells in the time course directly in the tissue. For this, a physiological property of the tissue was utilized, the so-called autofluorescence. Cells or tissue structures which are irradiated by light of a certain wavelength, start to fluoresce due to their biochemical properties. Thus, they become microscopically visible. In order to discern different structures, light of different wavelengths is used. When extremely short infrared pulses are applied, cells can be monitored in living tissue for hours. The resulting time lapse movies show for instance how immune cells communicate with each other (see link below this article).
In the aforementioned paper the technique was used in vivo in airways of mice and in living biopsy preparations of human lung tissue. Distinct cell types (granulocytes, fat cells, and epithelial cells) as well as tissue structures (blood vessels, epithelium, and connective tissue) were visualized without further staining. The migration of immune cells in the direction of an experimentally induced tissue lesion was observed in time course. Moreover, movement of granulocytes towards the site of an allergic inflammation was evident. No such movement was detected in absence of inflammation. Using antibody stainings, the spectrum of investigations was further extended: The researchers observed neutrophil and eosinophil granulocytes interacting with antigen-presenting cells. Cells of both types communicated on average for 13 minutes with each other. It is most probable that the immune response is modulated in this way.
This new technique offers further fascinating possibilities, but also poses some problems that have to be overcome first. For instance, fine structures like cilia can’t be visualized at present, as their autofluorescence is very weak. The state of cilia is important to know, because it might reveal the severity of a disease. Moreover, the image resolution in the living body isn’t as good as in fixed explanted tissue, because of body movements due to pulse beat and respiration. Dr. Gereon Hüttmann, Institute for Biomedical Optics at Lübeck University, thinks that this field holds a lot of potential: “Developments in the area of optical technologies promoted the telecommunication revolution and made their way into many sectors of our everyday life. They offer novel possibilities that we plan to utilize for medicine.” Scientists from ARCN work intensively on overcoming the obstacles. Prof. Dr. Peter König, Lübeck University, on the future development: “We are aiming at the visualization of cellular processes directly in the human tissue. We want to investigate diseases on the level of cells.” If this comes true in the long run, diagnosis as well as therapy of airway diseases will benefit from autofluorescence microscopy.
External link to this publication (open access)
Time lapse movies from the paper
/jbul
2024-04-24
2024-04-30
2024-05-29